Grief Blog






















Tip #6 Never Do This
Never Assume You Understand
Continuing the Series - Hospital Visit Tips, Never Do This…
6. Never Assume that You Understand
Maybe you had an aunt who had cancer or even your own cancer journey.
That does not mean that you completely understand what obstacles face every other person with cancer.
Even more painfully, just because your dad died doesn’t mean that you fully understand when her dad dies.
We can most certainly use our experiences to help us in lending support and compassionate care. But be cautious to put yourself in the role of expert due to your personal experiences.
Never say, “I know how you feel.”
Simply put, you don’t.
Just as no one can understand your personal grief or fear completely, you cannot understand theirs.
Instead, you could say, “If I were you, I might feel scared.” That communicates that you are trying to put yourself in their shoes.
If you are visiting with a patient and they share a concern or frustration, you might be able to reflect back to them. "You said that you feel like the doctor is not listening. Is there a nurse or advocate you could share those feelings with?"
By doing this we can help the patient take back their own voice and therefore enable them to advocate for and express themselves.
Never assume that you understand.
Tip #5 Never Do This
Never Disparage Clinicians
Hospital Visit Tip Number Five:
5. Never Disparage Clinicians
Disparage means to belittle or discredit.
I talk elsewhere about the danger of painting a medical situation as God versus the doctors.
While I encourage you sometimes to become an advocate for the patient, and even have hard conversations with clinicians, that doesn’t mean speaking poorly of them or vilifying them.
Remember that after you leave, those nurses, doctors, and other team members will continue to care for the patient. It’s best if we are all on the same team.
In my experience, I have never met a clinician who hopes for a poor outcome for their patients.
Therefore, never disparage the clinicians.
Never Question Their Faith Tip #4
Hospital Visit Tip Number Four:
4. Never Question Their Faith
People with serious illnesses or injuries are learning more about trusting God than anyone else. Suffering can have that kind of effect on the human heart.
No amount of belief in God can magically make a person healthy.
Reverend Ed Dobson, pastor and author, died of ALS (Lou Gerig's Disease) in 2015. In one of his last sermons, one he preached alongside his son Kent Dobson, he painfully addressed this common mistake.
Through extremely garbled speech due to the agonizing disease process, Dobson said, “People keep telling me to trust God. I want to ask them, ‘What do you think I am trying to do?'”
Please, never question the faith of the patient during a hospital visit.
Never do This - Tip #3
Never Interrogate the Patient
Hospital Visit Tip Number Three:
3. Never Interrogate the Patient
You don’t need to know every detail of their diagnosis, what medicine they take, how long they have had this disease, etc. We may be curious and this curiosity may show that we care, but now is not the time for interrogation.
Those details matter much less than you might imagine.
Resist the urge to ask if they have tried this or that remedy or treatment to regain their health.
Being admitted to the hospital involves a mountain of data and information.
No patient can be expected to remember it all and patients may become frustrated at their lack of memory.
Resist the urge to ask a million questions.
If we are honest, sometimes we ask questions to make sure that it couldn’t happen to us. Or someone we love.
That is a self-focused approach that won’t help the patient you see today.
Therefore, never interrogate the patient about their condition. Offering a listening ear about how they are doing in their heart and mind will communicate an important message; YOU are NOT a diagnosis or problem to be solved. You are a whole person in a place of suffering who needs to feel seen and heard, not questioned and frustrated.
Never do this - Tip #2
Here is the next installment of the Series “Tips on how to visit the hospital. 7 things to never do.”
Last week I introduced Number 1 - Never Force Prayer.
Prayer is a common response in times of suffering and crisis. However, for someone who is ill, in shock, or even questioning their faith, corporate prayer can be difficult at best.
So simply ask the person you are there to support if they would like prayer. Then respond accordingly.
2. Never Be Afraid to Cry
When people hear what chaplains do, they ask some common questions.
One common question is, “Do you ever cry when you are serving a family whose loved one just died?”
The answer, of course, is yes.
The day that violence, suffering, sickness, cancer, miscarriage, stillbirth, strokes, heart attacks, and death can no longer bring tears to our eyes is the day we should quit being hospital chaplains.
While it is important that I don’t make the situation about myself and my own sadness, shedding some tears with the family can build a meaningful bridge.
I can vividly recall a friend who responded to me in a time of great pain and suffering with a few but deeply felt words. "I am crying with you!" Just knowing that our pain is seen and felt by others brings great comfort.
I no longer apologize for crying, and neither should you.
Never be afraid to cry with the hurting.
Never do this when you visit the hospital Tip #1
Visiting the hospital can be intimidating. How can you be sure to help? Follow my "Hospital Visit Tips."
1. Never force prayer
Should you pray for people in the hospital? Of course.
If you are a person who prays, you should pray for people in the hospital.
However, should you pray out loud and in person?
It depends.
Here’s how you can decide. Simply ask if they would like a prayer.
In my experience, you can expect one of three responses.
1. They say, "Yes," and shift in their bed. That means they want you to pray out loud and in person, and you should do it now.
2. They say, “I’d be happy to be on the prayer list,” or “Keep me in your prayers.” That means they don’t mind the idea of prayer, but they don’t want to do it now.
Maybe they aren’t feeling great, are tired, or want to call the nurse to help them to the bathroom. In that case, it’s time to leave, and you can pray as you walk out of the hospital.
3. They ignore your question about prayer altogether.
This might indicate that they are struggling with what to think about God while they are sick or injured.
For this group, forcing prayer could be a big mistake.
Think of it this way.
Kristen and I have four children. When they were young, they would often hurt or offend one another, as siblings do. Their mom and I would force them to apologize to one another. However, you can imagine how those forced apologies usually went. They were quick, insincere, and usually still full of anger and frustration.
Did the forced apology reconcile the relationship? No.
And forced prayer doesn’t improve the patient’s relationship with God, either.
It can do damage.
That’s why you should never force prayer when visiting a patient in the hospital.
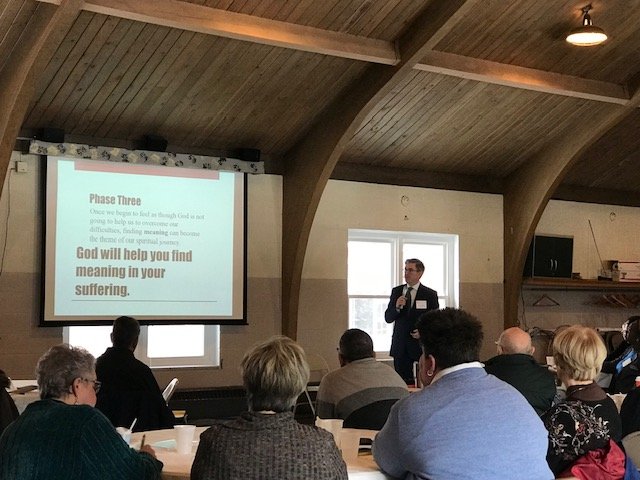
Upcoming in person event
Join me on Thursday, August 24 for a day-long workshop hosted by the Center for Congregations. This workshop will be held at The Summit Event Center from 9:00 am-4:00 pm.
When faith communities encounter death and grief, they have intense questions. These questions may deeply impact their faith journey. What is your role as a leader? How can you best guide your congregation through loss, death, and grief?
Sickness and death are certainties, but when accompanied by good pastoral care, they can be the cracks through which the light of faith and hope can shine.
During this session, you will:
Examine case studies of congregants facing death and grief and role-play examples
Learn how to help your congregation balance faith and fear during times of health crisis, including practical considerations for hospital visitation
Practice completion of medical directives
Learn the best pastoral practices as you care for the sick, dying, and grieving
Consider your own grief, anxiety, and fear of death
Phase Three
Phase Three - it’s time to change the conversation.
In previous newsletters, we talked about Phase One (primarily focused on the future), and Phase Two (working hard to overcome present difficulties).
But the cliches of Phase One and Two don’t work for people in Phase Three. In Phase Three we face difficulties that cannot be overcome. In Phase Three finding meaning is what matters most.
Phase One is about Plans.
Phase Two is about Overcoming.
Phase Three is about Meaning.
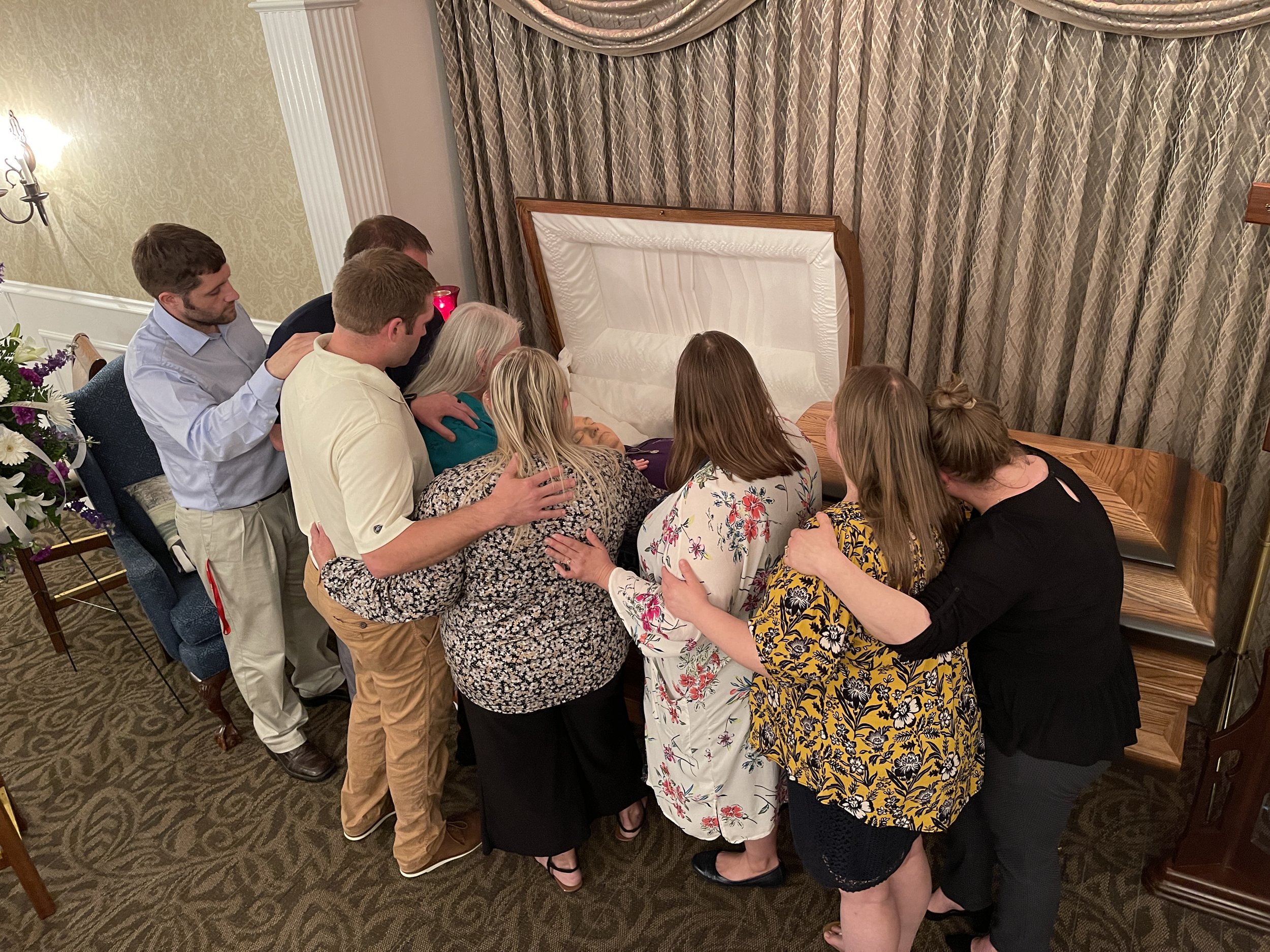
Think about how you felt at the last funeral you attended. Or when someone close to you died. This isn’t difficult for me. This photo was taken at my Father In Law's funeral, in May 2021. Dan was a beloved husband, father, papaw, teacher, and coach. Here he is surrounded by his wife of 46 years and his seven children.
My focus wasn’t on making plans for the future or getting stronger by overcoming that devastating loss-we never will overcome it this side of Heaven. My focus was on what mattered to Dan, in his life and death, and those closest to him, including my wife and my children.
99% of our life experiences are in Phases One and Two.
But to a griever, 100% of life feels like Phase Three.
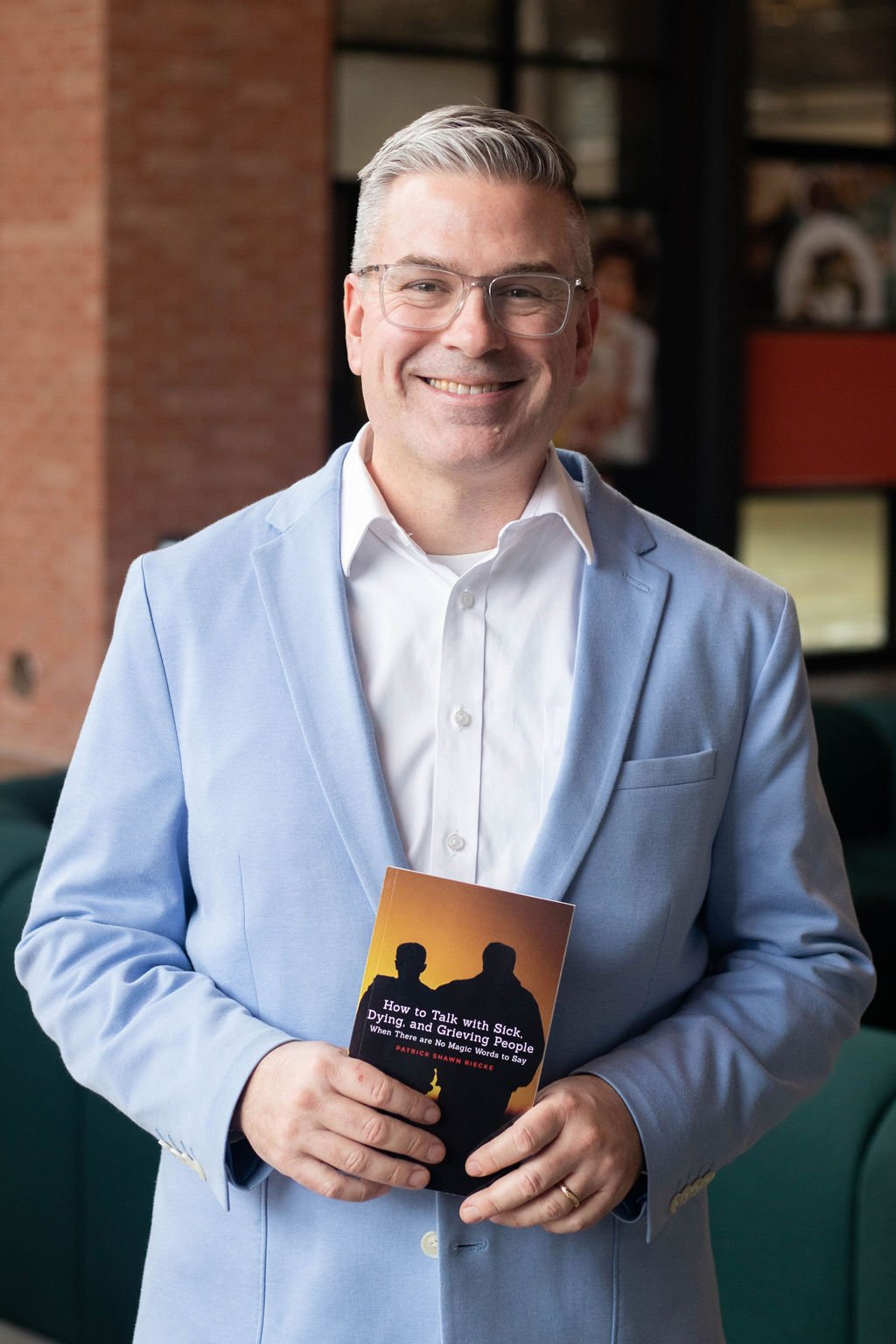
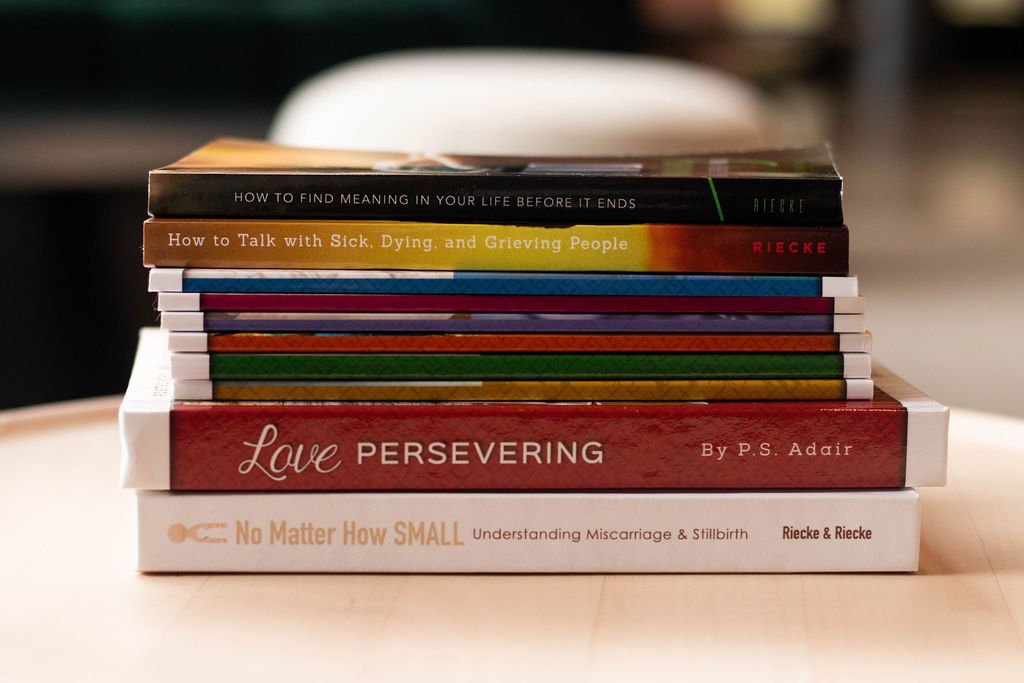
This is why the conversation needs to change in Phase Three. For guidance and practical advice on how to do this well, pick up How to Talk With Sick, Dying, and Grieving People today!
Phase Two
In the previous blog, I talked about the "Three Phases of Life."
Phase One is future-focused and is a launching point for our lives-
both physically and spiritually.
Today let's talk about Phase Two, where we spend most of our life if we are lucky!
Phase One is all about the future--good things are coming.
God has big plans for you, hope for a future full of potential.
Picture that high school graduate about to take the world by storm.
The problem is that a new graduate isn’t going to take the world by storm.
But life will send plenty of storms his way. He will need to overcome those storms. And that’s what Phase Two is all about overcoming adversity. In life, we face one problem after another. We rely on ourselves, God, or others, and hopefully, a combination of the three, to help us overcome those problems. When faced with challenges in our present-day culture, we are encouraged (often demanded) to "deal with it" or "man up." Because, after all, whatever doesn’t kill me makes me stronger.
If pain is weakness leaving the body, then each obstacle we face is an opportunity to get better and stronger. While I’m not hiding my opinion that this phase doesn’t help grievers, one thing is true: This is an incredibly helpful way to view our lives.
After all, we can’t let our problems routinely defeat us.
So then, what’s the problem?
The problem is that some obstacles can’t be overcome.
Luckily, when our first baby died, no one said, "Patrick, just deal with it!" Or, "Don’t cry! This pain will make you a stronger parent."
How do we describe the phenomenon when we can’t get past an obstacle? At least not in the way we had hoped. This is when we are faced with what Viktor Frankl calls a “fate that cannot be changed.”
This unchangeable fate is more common than we would like to admit.
It’s called Phase Three.
How to Talk With Sick, Dying, and Grieving People
If you want to understand how to navigate your own grief better or to support those struggling to process their grief. Click on the link above and pick up the paperback, audible, or Kindle version of my book on Amazon today.
Three Phases of Life
My first book, How to Talk with Sick, Dying and Grieving People: When There Are No Magic Words to Say, was a total outpouring of my heart. That book is built around "Three Phases of Spiritual Growth" but could easily just be called “Three Phases of Life." I am introducing the first one below!
Phase One
Phase One’s theme is “The best is yet to come.”
It's completely future-focused.
Picture a high school graduate, clothed in a cap and gown.
The whole world is before him. Oh, the places you'll go!
It can even be quite spiritual. People of faith love new beginnings. Who doesn’t?
The mantra in this phase is...
“God loves you and has a wonderful plan for your life.” It's the prevailing theme of vacation bible school and Sunday school curricula around the globe!
The theme verse is “‘I know the plans I have for you,’ declares the Lord, ‘plans to prosper you and not to harm you. Plans to give you a hope and a future.’” Jer. 29:11
It’s a good place to start. And I believe it. So, what’s the problem?
Well, imagine reciting these phrases to a griever:
“The best is yet to come.”
“God has a wonderful plan for your life.
“Focus on the future.”
At best, that’s tone-deaf to their pain.
At its worst, it sounds downright cruel to a broken heart.
That is because the griever is in Phase Three! Follow along as I highlight the three phases from my book in the next three weeks, via my newsletter.
If you can't wait for the upcoming emails, click the button below. You can purchase the Kindle format via Amazon today for only $0.99!
Two Years Later
[Note: This week is the two-year anniversary of this story. And it still feels unbelievable.]
In my 20’s I was a youth minister for eight years at two different churches. I was always fortunate to have volunteer youth sponsors who not only mentored the kids in the youth group, but mentored me as well. These sponsors were mostly older than me, and often had their own kids in the youth group.
Mike Maxson was one such volunteer. Long before I knew Mike, he was an alcoholic and maybe a drug user, but I don’t remember. When he served with me in youth ministry, he was an addictions counselor, ran the sound for our youth worship band, and always took time off work to go on retreats and camps with the high school youth group.
Mike’s daughter, Bre, was one of our favorite kids in the youth group. We first met when my wife, Kristen, and I taught her fourth-grade Sunday school class in the year 2000. Even after I moved on from that church and Bre graduated from high school, we all kept in touch.
Many years later, after I started working as a Chaplaincy supervisor at Parkview, my phone rang. It was Bre Maxson, now a college graduate engaged to a wonderful young man named Joshua Vire.
“Patrick, I think you know that my dad’s in the hospital,” She said.
I did. In fact, I had already visited Mike a few times, but missed Bre and Josh.
“And you know that Josh and I are getting married this fall, right?”
I did. And I joked with her that I was offended that she hadn’t asked me to be the officiant, but opted for a friend of mine named Ben.
“Well, we might have an opportunity to fix that for you. You see, they are saying dad doesn’t have long to live. He’s full of cancer. In fact, he might not make it to our wedding date in October, just four months from now. Would it be possible for you to perform a wedding ceremony for us at Parkview?”
At three o’clock that afternoon, my favorite wedding as an officiant occurred on the 7th floor of PRMC.
RTs, RNs, OTs, nutrition services, EVS, and others collaborated to make a beautiful spread including a linen tablecloth, fresh flowers, and a white-iced red velvet cake in Mike’s room.
Mike gave Bre away and weakly signed as witness on their marriage license.
Four months later, due to some great work from our Palliative care team at Parkview, Mike was still alive, although still full of cancer. He managed to stand up from his wheelchair just long enough to dance with Bre at their previously scheduled (non-hospital) wedding ceremony.
A couple of years later, Mike died with dignity in his home, supported by home health and hospice. This time, with many of the same people in the room, I officiated a funeral instead of a wedding. It was sad and holy. Awful and awesome. Horrible and honorable.
But that’s not the climax of the story.
Bre and Josh were happily married for five years, but also burdened with infertility. After many doctors’ appointments and failed attempts to start having children, they decided on embryo adoption. Shortly after the world locked down in 2020, Bre became successfully pregnant for the first time. They were thrilled and we were thrilled for them. We kept in touch regularly and attended our first baby shower to be hosted on zoom. Josh is a childhood cancer survivor, and Bre was delicately pregnant, so they committed to a life of isolation until the baby arrived.
In March of 2021, near the end of Bre’s pregnancy, Kristen got a voicemail from her. Bre asked if Kristen could pick her up and take her to an appointment, since their vehicle was low to the ground and hard for her to use so late in pregnancy. But Kristen and I were in Puerto Rico on a vacation, so Kristen texted her in reply and they made plans to connect upon our return. Little did we know what that connection would actually look like.
We got home late that Friday night and went to bed, laden with Dramamine and after-travel fatigue at about midnight. At one o’clock in the morning, my phone rang. It was Chaplain Jana Vastbinder, and she was working overnight at PRMC. This is what I heard.
“Patrick, I know you’re not on call. But this is about Bre. She’s here at the hospital. The baby is fine. But Bre is not. Patrick, Bre is coding in STICU right now. Josh wants to know if you can come.”
Ten minutes later I walked down the STICU hallway. More than thirty staff members rushed in and out of Bre’s room, and Josh sat helplessly behind the nursing module.
Baby Judah was taken via c-section by Dr. Freyre and her team, and now the trauma team, cardiology, and the ECMO team were in full sprint. Bre’s lungs had been assaulted by three massive blood clots.
The CODE team rode Bre’s bed all the way back to surgery. The clots were removed, she was placed on ECMO, and everything was done that needed to be done.
In the middle of the night, I realized that baby Judah was in our Family Birthing Center with no mom and no dad because Josh was rightly staying with Bre. No grandparents had arrived yet, and no other family. So, in the middle of a pandemic, while his mom was in the fight of her life, Judah was born into the world to the herald and love of only Parkview coworkers. My wife, Kristen, served patients in our Family Birthing Centers when they experience stillbirth. She had a badge and great relationships on the unit. I asked one of the FBC nurses if she knew Kristen. She did. I asked if she thought the nurses would let Kristen on the floor to be a surrogate family member until others arrived. She did.
There are more details than I have time to recount but permit me one snippet. Late Saturday afternoon, after Bre’s brain death had been declared and shared, after I poured out an angry out loud prayer to God while four physicians, the ECMO team, and PHI nurses all bawled our eyes out, after chaplain Will and chaplain Dan held me as I convulsed in tears, but before Josh said his final goodbye to his bride on this side of Heaven, baby Judah made his first sojourn. Plump and perfect, he left the FBC in the care of RNs and Kristen. When I returned after a short time at home, Judah was snuggled up to his unresponsive mother. He leaned into her shoulder and cheek, not caring one bit that she was intubated and sustained by a huge and loud ECMO machine. As I stood outside the room I noticed that Parkview Public Safety Officer Tyler hadn’t left the nurses station, right across from the door to Bre’s room. Then the penny dropped for me. Judah had his HUGS tag removed when he left the FBC so the alarms didn’t sound. Someone decided that meant he needed a police escort.
I leaned across the desk, close to officer Tyler. “When you came to work today, I bet you didn’t expect to be security detail for a baby born yesterday, did you?”
“No sir,” he said. “But it’s an honor.
A week later, on Easter Saturday, I was an officiant again. This time, not for Bre’s hospital wedding. Or her dad’s funeral. But for Bre’s funeral.
Many PRMC nurses and doctors came, cried, supported, and loved.
Just over a year later, Judah is a bouncing baby boy who has just learned to walk.
Usually, I don’t really like babies that much, but Judah. Judah is different. He’s special. He’s… perfect.
You see, this is part of what it means to work at a hospital.
It means that you get to see some of life’s most beautiful moments. Birth of a new baby, recovery from injury or illness, reconciliation of family and friends.
And you see some of the worst things in life. Abuse and trauma. Death and destruction. Loss and grief.
It’s never been either/or.
It has always been both/and.
In fact, this is also part of what it means to be human, let alone a healthcare worker.
Today, as you live in the tension of pain and joy. Hell and hope. Dignity and despair. May your heart be expanded enough to make room for it all.
Because in the same building, a linen tablecloth is spread for an impromptu wedding, and a baby meets and says goodbye to his mother on the same day.
Open your heart to the pain. And open your heart to the joy.
Bucket List Living
In October 2019, Parkview Health executives invited Ben Nemtin to deliver a keynote speech.
His presentation changed my life.
His central question is, “What do you want to do before you die?”
“At the end of their lives, more people regret the things they didn’t do, than the things they did do,” Ben explains.
Over the last ten years, I have led the Parkview chaplaincy team as they have responded to more than 14,000 patient deaths. We had a front-row seat when many of our citizens arrived at the end of their earthly journey.
So, I know that Ben is on to something.
But for me, there was one big problem. This question feels, I don’t know, selfish.
As a Christian Pastor, I have lived my life with a certain (incomplete) framework.
My mental script has gone like this:
“What is the right thing to do?”
“How can I be more selfless?”
“What does the world need and how can I deliver it?”
Perfectly fine questions and I believed I was pleasing God with this framework for my life.
However, it has had some negative outcomes.
Living my life through the lens of “should” instead of “want” has led to:
Frustration (with myself and others)
Trying to control (myself and others)
Shame (when I did something wrong)
Resentment (when things didn’t turn out the ‘right’ way)
Last year, Ben came out with his new Bucket List Journal. I was still living with frustration and shame. Even so, I preordered a copy of the journal. The next week, Ben returned to Fort Wayne, speaking for a fundraiser for Erin’s House for Grieving Children. My wife and I arrived early, visited with Ben, and enjoyed his talk.
It was time to start making my own bucket list. Could it help me adjust my framework so I felt less shame and resentment?
Tentatively, I started compiling my list.
Here are a few items I have included:
48. Visit the Holy Land
65. Attend an Indiana University men’s basketball game at Simon Skjodt Assembly Hall in Bloomington
5. Have lunch with Ben Nemtin 😁
36. Be a keynote speaker for an event outside of the United States
Here are a few that I have already crossed off:
60. Boil a tea kettle until it whistles (yes, I lived to be 44 years old and had only seen this on TV)
18. Own a three-year supply of firewood
58. Set up a nice, quiet home office
11. Work with a financial advisor
The list is great. And it’s starting to make an impact (even though I am still a Bucket List novice).
In fact, the list might be decreasing my shame and resentment.
Item #18 (above) is a perfect example.
“Own a three-year supply of firewood.”
Last summer, I added this item to my bucket list. Then, I noticed that my neighbor had a huge supply of firewood. It ran the length of one side of his house, and they didn’t seem to use it. But I don’t know this neighbor very well. Even though we have been neighbors for years, we’ve never struck up a friendship.
And I feel guilty about that.
Every day last summer, I planned to ask him if I could buy some of his wood. It would be a lot easier than transporting that much wood from someplace else.
I saw him from time to time. I wanted to ask. But I kept chickening out.
This is what was going through my mind:
The right thing would have been to be a better neighbor. But I haven’t done that. I felt ashamed. Why would he care if I wanted some easy-to-transport firewood? In fact, he probably hates me because I haven’t been the neighbor I should have been.
See what I mean?
Living with the framework of solely trying to do the right thing led to shame, distance, and an extreme lack of firewood.
The lie I believed was that my desires don’t matter.
Once we believe that lie, it’s a small leap to the next lie. The lie that I don’t matter. Which, by the way, is a profound violation of the message of the New Testament. I have two degrees in the New Testament. So, you would think I would have learned this lesson already.
One day, I was mowing the lawn. I had my shirt off, which is kind of gross and probably the wrong thing to do for a man my age. Just then, my neighbor appeared out of his garage.
I swallowed hard and ignored my inner critic telling me I should keep my mouth shut since I am a bad neighbor.
I let go of the mower handle, killing the engine.
“Hey, Bob (not his real name),” I stammered. “Uh, I was gonna buy some firewood, so I thought I would. Well, I wonder. Would you mind selling me some of yours, if you don’t mind?”
I swallowed hard again. I felt like I was speaking a foreign language. The language of “want” instead of the language of “should.”
He didn’t miss a beat. Probably because he hadn’t rehearsed this interaction in his head a hundred times as I had.
“Oh, take as much as you want. We don’t use it.”
“Ok,” I gained a little confidence. “Would $50 be enough if I took about half of it?”
“You don’t need to pay me anything, you’re welcome to it,” he said.
“Thanks,” was all I said.
But what I meant was, “This crosses off number 18 on my bucket list of things I want to do before I die. It was SUPER hard for me to ask you this, but now I feel so affirmed that living this way is really possible. I feel free and unashamed; like I am worth it! I am valuable enough to have a three-year supply of firewood. Thank you, Bob, thank you!”
Upon reflection, it’s probably good that I didn’t say all of that. He would have thought I was nuts.
Reframing my life as an adventure where I get to do things I want to do (before I die) is having the following effects:
1. Increased Energy
Pursuing something I want is more energizing than avoiding a wrong action.
2. Inspiring Others
I signed up for an online course called “Travel-Hacking” to become a more knowledgeable traveler (bucket list item #57). Immediately, I texted our four kids. They replied, and I quote, “Yessirrr,” and “Let’s go dad 🐐.” The goat emoji means “greatest of all time.” That might be an overstatement.
3. Increased Gratitude
I look at my pile of firewood often. I sit in my new quiet home office and I feel deeply thankful. These are things I wanted. Now I have them. And I thank God.
4. Decreased Shame
Nothing busts shame and resentment like crossing something off my list!
5. Desire-Affirming
I find joy in crossing things off my bucket list.
Recently, I again mustered the courage to ask for help crossing an item off my list. In response, the young man working behind the counter clickety-clacked the keyboard. His name tag read that he was from India and his name was Joe. In a few swift movements, he granted my request with ease. My eyes brimmed with tears of joy.
“Joe,” I said in a solemn voice. “Do you know what a bucket list is?” He gave a confused look at first. “A list of things you want to do before you die?” I asked. Then his face showed recognition.
With tears, I said, “You just helped me cross an item off my bucket list.” I stared into this stranger’s eyes for an uncomfortably long time. “Thank you.”
“You are welcome, sir, very welcome. Thank you.” Joe’s eyes got a little glassy as well, knowing he made a difference in this random stranger’s life.
How about you? What do you want to do before you die?
Do you have a bucket list?
Are you worth it?
Could you start one today? Record it on paper or a note on your phone.
What’s the next step for you to pursue your desires?
Damar Hamlin, Bills Safety
I wrote this on LinkedIn Monday night after the 24-year-old defensive player went down, received CPR, and was transported to a local hospital…
If you are watching Monday Night Football…
You’re seeing the response we see so many times at the hospital.
Not just the CPR.
Not just the medics.
Not just the hospital, intubation, and updates that are agonizingly slow to arrive.
But also the terror of the people close to Damar Hamlin.
The inability to string words together, even for professional broadcasters.
The sense that we need to do something (#DamarHamlin's charity has received nearly $7M since Monday)
Panic.
Sobs.
And support.
Prayers for the Buffalo Bills player who went down tonight.
I hope he makes it out okay.
I’m sorry
Christmas
If you are grieving someone, today and tomorrow might be hard for you.
Recently, I talked with a dad about his daughter. My heart broke for him. Before we hung up, I asked if there was anything more I could do for him.
He choked up and said, "Not unless you can bring her back."
"I wish I could," was all I could say. "I'm sorry."
I wish I could heal your heart. I cannot.
I'm sorry.
Anne Lamott said, “You will lose someone you can’t live without, and your heart will be badly broken, and the bad news is that you never completely get over the loss of your beloved. But this is also the good news. They live forever in your broken heart that doesn’t seal back up."
Love perseveres.
If you're looking for a cozy fiction book over the holiday, you'll love the Postscript Book Series. I wrote these under the pen name "P.S. Adair."
Six short grief-centered stories. About an hour each. Paperback, audio, hardcover, or Kindle.
WARNING: They will probably make you cry
Grief and the Holidays
What To Say to a Grieving Person during the Holidays
During the holiday season, grief can be even more daunting. What do I say to my friend/patient/member who is sad about a death this holiday season?
It can be helpful to say: "You Have Options"
Grief constricts. It can feel tight. Like you are tied up.
But holidays present opportunities. While most people dread the first year full of holidays, we also have the option to remember the person who has died purposefully. Giving the griever options is a loving act that can set them free.
They could:
1. Purchase an ornament to remember their loved one
2. Have a moment of silence to remember them at a family event
3. Adopt one of the traditions that person enjoyed (they could make the pie this year)
4. Go to a "Blue Christmas" service or another memorial service that remembers those who have died
5. Make a charitable contribution in their memory
6. Decide it's okay to forgo past traditions this year
Giving grieving people options might be the best gift they get this year.
My good friend, Dr. Jon Swanson, wrote on this topic recently, too. Click here for his blog.
What NOT to say to griever (Tip #6)
6. At least…
Kate Bowler calls this “brightsiding.” It comes in many forms.
At least you got to say goodbye.
At least you had a lot of years together.
At least you didn’t have time to get attached.
At least you know where she’s going.
At least it was quick.
At least you had a long time to prepare.
At least you still have other living children.
This cliché, like others, does two hurtful things. First, it minimizes the grief of the griever. Any statement that begins with at least puts two realities on a scale.
On one side is their loss. On the other side is whatever reality with which the at least statement concludes (e.g., other living children, many years, the promise of heaven, etc.).
The implication is that there are realities that could outweigh their grief.
However, if you have ever carried real grief, you know this isn’t true.
Second, at least comments are trying to fix a situation that cannot be fixed.
After all, if I can convince you that the promise of heaven is greater than the pain of grief, you’ll stop being so sad, and I’ll feel like I solved your problem.
If you are about to say “at least…”, instead try, “does it help that…?” Does it help that you had a long time to say goodbye? Does it help to think about them in heaven?
That makes the griever the expert, and invites them to talk about their feelings.
What NOT to say (Tip #5)
5. God must have needed them more than you do
This one has similar problems to "God needed another angel in heaven."
It cuts in two ways.
First, it paints God as selfish during a season when the griever needs God to be caring.
Second, it minimizes their connection with their loved one.
So, don’t say “God must have needed them more than you do.”
What NOT to say to a Griever (Tip #4)
4. Time heals all wounds
This is the kinder counterpart to the previous cliché (“Move on, it’s been a long time”).
The problem is, this sounds almost right.
But consider this.
Do you know anyone you might describe as "stuck" in grief that happened a long time ago, maybe even decades? If so, has time healed all wounds? No.
It is certainly true that time can change grief's complexion, but time does not heal all wounds.
In fact, grief can suddenly pop up many years later, as fresh as it was at first.
Tip #3 What NEVER to say to a griever. “You need to move on. It's been...”
In 1969, Elisabeth Kübler-Ross published her book On Death and Dying. Out of that book came the famous "five stages of grief."
Kübler-Ross never intended to portray grief as a straight line from denial (the first stage) to acceptance (the fifth stage). However, she has been interpreted in this way.
The result? People think you must move through the stages sequentially, linearly, never doubling back, and always moving forward until you are... done.
Recent experts on grief have taken serious issue with the notion of linear movement through a "grief process."
Grief is more adequately understood like a toddler's scribble instead of a straight line from stage one to stage five. The line switches back on itself, covers territory many times, takes sharp turns with no warning, and never ends.
Therefore, please never suggest that a grieving person should move on after a certain amount of time.
For more tips on how to:
Eliminate hurtful practices
Improve retention
Increase engagement,
Step #2 to help Grievers
Go!
The most ancient part of the Hebrew scripture focuses on death, dying, and grief.
The book of Job (pronounced with a long “o”).
Job’s family and friends all died--in one day. He lost everything except for his wife and a few friends.
Our story picks up when the friends come to visit Job.
They did five things right, initially.
They:
Made a plan
Went to see Job
Sat down
Were silent, and
Wept out loud
In this email, let’s unpack their second right move.
They went to see Job.
They didn’t add him to the prayer line.
They put a full stop to their ‘normal lives’ for their friend. They left their own homes. They decided to be with their friend on purpose.
When I was in Bible College, I lived nine hours from home. I was in the student center one evening when Ryan (my roommate, and not his real name) came in.
I could tell something wasn’t right.
Ryan and his grandfather had a close relationship. One of those “go out to lunch, just the two of them” type of friendships.
Ryan had just gotten off the phone with his mom. She shared that his grandfather had a medical event and was in the hospital. They were moving him to comfort care and his death was imminent.
Ryan was devastated.
He wanted to see his grandfather. But our finals were just a couple of days away. It was a long drive and his mother had encouraged him to stay at school.
“What do you want to do?” I asked.
“Well, I want to go… but…” he responded.
“Then let’s go,” I said. A college kid is always up for a sudden adventure.
A small light dawned in his eyes. “You mean, both of us?”
“Sure.” I smiled. “I know how to get there…” (We grew up in the same hometown.)
Ryan took me up on the offer, and in twenty minutes we were in his car and speeding out of town. We encountered exactly zero troopers on our 455-mile trip, which was good for us. A trip that usually took us nearly nine hours was completed in six hours and thirty-nine minutes.
I dropped Ryan off at the hospital and went home and fell asleep.
The next day my phone rang. Ryan was on the other end. His grandpa died just a few hours after we arrived in town. He was thankful for those hours.
Sometimes you just need to go.
Job’s friends went.
Sometimes the best way to help is to put the rest of life on hold and go.
If you are a part of a group that would like to have a grief talk, click the button below.