Grief Blog






















Faith vs. Medicine
God vs Docs
Sometimes people can portray medical situations as ‘God vs. the Doctors.’
People of faith may feel at odds with the clinical team.
Have you ever heard people say things like this?
“The doctors don’t have the final word.”
“God will decide when I am going to die, not the doctors.”
“People all over the planet are praying for my dad. I know that prognosis can’t be true.”
While these feelings are genuine, they lead to a dangerous dichotomy. It can seem as if it’s some kind of competition where only one (the doctor or God) can win.
But when we gather around a hospital bed, painting the situation as God vs. the Doctors doesn’t help anyone.
Some people think that most physicians are anti-faith or atheists. Of course, that’s not true. A 2005 study discovered that doctors in the United States are people of faith at a rate that is nearly identical to the rest of the population.
When a doctor tells you that she or he thinks you are going to die—they hope they are wrong, too.
Doctors don’t wish for patients to die.
Quite the contrary.
Dr. Atul Gawande is quite vulnerable on this point in his book, Being Mortal. Physicians usually err on the side of doing too much to save a person’s life and being too optimistic, not the other way around. Estimates of patient survival given by physicians (e.g., “you have six months to live”) are heavily influenced by the optimism of the physician.
In one study, researchers discovered that while the physicians’ prediction of survival (of cancer patients) averaged 42 days, actual survival averaged only 29 days. That means that the physicians were holding out more hope than warranted, not less.
Many believe this overestimation of survival is the result of the emotional struggle many physicians feel when discussing patients’ prognoses with them. Imagine being the person who tells a family that their loved one is going to die in less than a year or less than a month.
The point is this—no matter the faith, the people skills, the tone, the education, or anything else—the doctor wants the best possible outcome for every patient in every situation. They are hard-wired to want this so much that they usually cannot bring themselves to admit how long (or short) they think you will live.
It does not help anyone to paint the situation as God vs. the Doctors. If I am a patient in a hospital bed with a scary diagnosis or injury, I need to feel that everyone is on my side—my family, my faith community, and my clinical care team.
If you are a part of a group that would like to have a grief talk, click the button below.
How to Visit the Hospital (always do this)
Always do this when you visit the hospital
Keep it Private
Not only does HIPAA federal law prevent you from sharing protected health information, but it’s also a matter of respect.
I’m sorry to say that I have often heard leaders tell very intimate details about a person’s health when they should have kept it private.
Better yet, ask the person or family member:
If they want their team at work to be updated on their health
If they want to be placed on a prayer line
How they feel about others knowing
If the information is public (on social media, etc.).
Treat their information like you would the news that a woman is pregnant.
It’s her news to share with whom she so desires and when she desires to share it.
Patients deserve the same treatment.
Don’t take that right away from them.
If you are a part of a group that would like to have a grief talk, live or online, click the button below.
New Fiction Released!
Lori has had a hard life. Her childhood got off to a good start, but after her mom died in a horrific car accident, life was never the same. Her dad became angry and abusive, and he made Lori feel like she was worthless.
Even in adulthood, Lori's self-esteem was horribly low. That's part of why she married Jeff--a man just like her father.
On that foundation of abuse and toxic relationships, Lori experienced the most brutal grief in the world--the death of her child.
In a tailspin, will Lori make it out alive? Will she get the help she needs? Will she ever stand up to Jeff and find a way to use her writing career to help mothers like her?
Lori's Voice is a painful yet inspirational story. Read it today to have your heart broken but your soul inspired by the strength Lori finds.
This is a short read--about an hour in length.
One Hour Online Seminars
ONE HOUR ONLINE WORKSHOPS
More people have died in the past two years than ever before. It's a statistic, but also a reality that people are experiencing right now.
Think about the grief around you.
Coworkers.
Friends and family.
Clients, patients, and members.
You want to help, but it is overwhelming.
You can do this.
We can help.
Schedule a One Hour ONLINE workshop today!
For groups from 5 to 500
Limited time introductory price, so act now.
Become the friend, leader, the team that grievers deserve. This workshop will transform you from feeling overwhelmed to being prepared.
Click the button below and complete a 2-minute questionnaire to plan your workshop.
P.S. Don't worry about the details: price, schedule, technical requirements. We will work together to make a plan that fits what you need so that you can be prepared to help grieving people.
New fiction released!
Toby and Jayda were high school sweethearts, and as a young married couple, they were just finding their way.
Nothing could have prepared them for what happened next. After their daughter died, Toby felt angry, then sad. Finally, he felt stuck. His mentor, Pastor Thomas, was no help--he made everything worse for Toby. Toby hasn't even painted in months. That was Jayda's signal that he was stuck in a dark place.
Can Jayda help Pastor Thomas see the light? Can Toby get unstuck and paint again? Will this sweet young couple survive a devastating loss so early in their lives?
A tender tearjerker, Toby's Daughter Died will break your heart and is only an hour-long read. You'll fall in love with gentle Toby, and loving Jayda.
Read this story today with a box of tissues nearby.
Do you have a friend who devours fiction? Forward this email to them today.
Don't forget to leave a review and let me know what you think! I'm totally new to this, and it's been a passion project, so I would love to have your feedback.
Cheer up!
These mistakes are like gravity. Even experienced caregivers are pulled towards committing these cardinal sins.
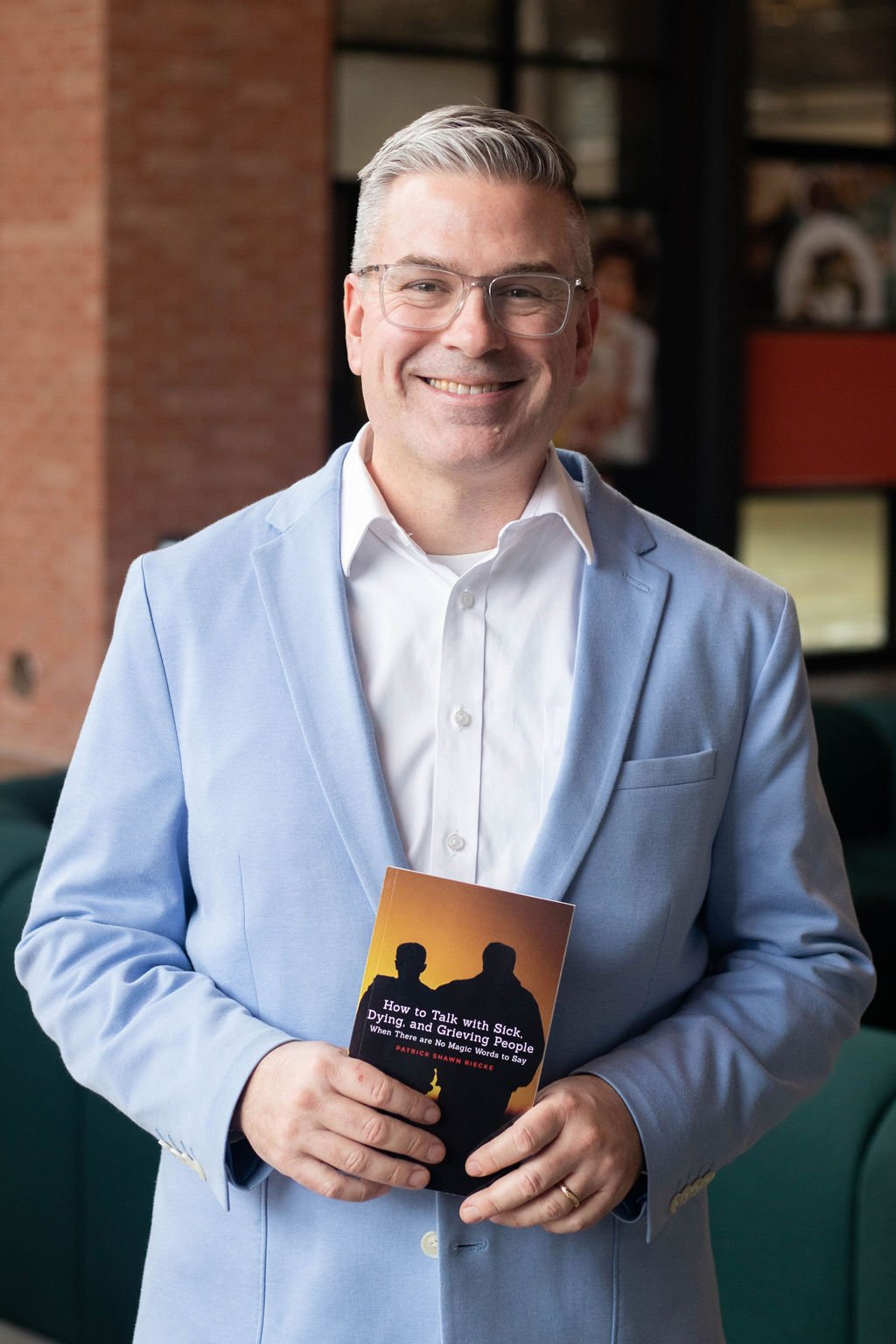
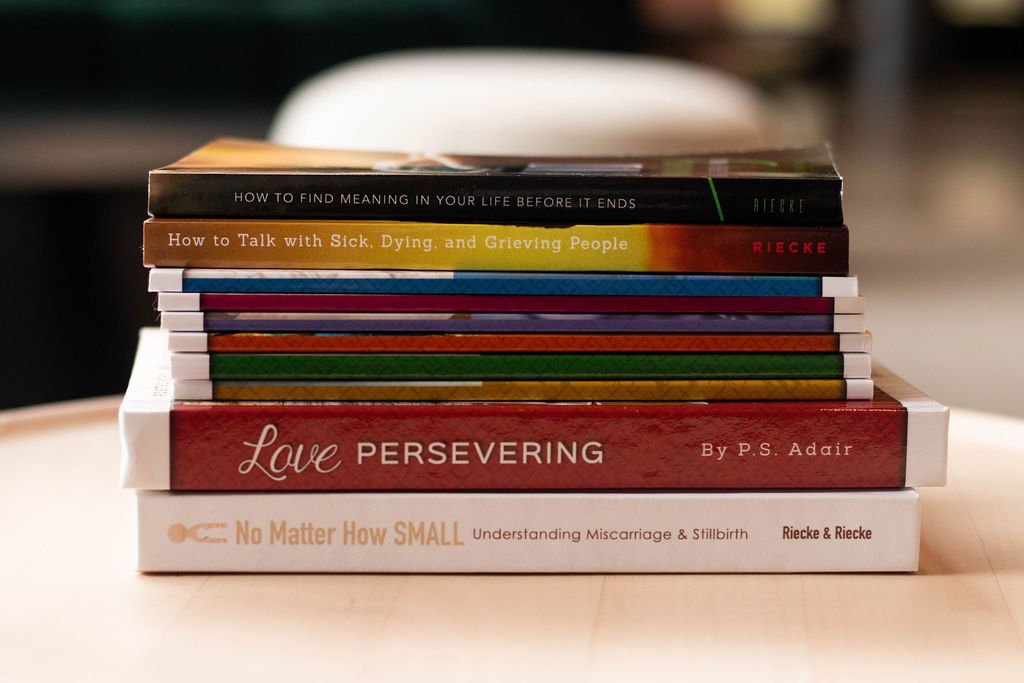
In my book How to Talk with Sick, Dying, and Grieving People: When There are No Magic Words to Say, I list them all. Today, let me share just one common mistake that tempts so many of us.
4. Cheering people up
Young people usually understand the emotional nature of difficult times better than older adults. I remember a young man who was a part of my youth group years ago. When he learned that his friend’s mom had died, he told us all he just wanted to punch the wall. Then, at the funeral service, he stood with his friend over to the side, just talking, and laughing.
That kind of ebb and flow of emotions is natural during grief.
Don’t try to cheer people up. Just ride the waves of emotion with them.
If they are sad, let them be sad. If they are happy let them be happy!
Only Focusing on the Afterlife
Some mistakes are like gravity. Even experienced caregivers are pulled towards committing these cardinal sins.
In my book How to Talk with Sick, Dying, and Grieving People: When There are No Magic Words to Say, I list them all. Today, let me share just one common mistake that tempts so many of us.
Mistake #3. Only focusing on the afterlife
Let me tell you a story.
For several months, our daughter was haunted by night terrors.
Not simply nightmares, but night terrors.
If you have ever seen someone have a night terror, you know the difference. It’s a combination of sleepwalking and a nightmare and multiplied by ten.
Each night, a couple of hours after we put her to bed, she woke up screaming hysterically. She would repeat one or two words, usually “Mommy…” followed by another word or phrase.
At first, we tried to wake her up and tell her everything was ok. Every time she called for us, we asked “What is the matter, sweetie?” Sadly, she could never respond to our attempts to communicate.
We bought a camera for her room so we could see what was causing all the chaos.
The answer? Nothing. There was no cause.
She just woke up with tears flowing, chin quivering and arms flailing.
When we learned about night terrors, we changed our approach.
We no longer tried to dialogue with her. We didn’t get as frustrated with her. We didn’t ask her what was wrong. We just tried to be close to her, give her what she needed, and wait it out. Usually, in about ten minutes she went back to sleep. She never even remembered those events the next morning.
Trying to convince my daughter that ‘everything was okay’ during these episodes is similar to trying to tell a griever that everything is okay because their loved one is in heaven. It might be true, but it’s not effective.
It's not that we can't focus on the afterlife at all, but we can't focus SOLELY on the afterlife.
After all, it's Christmas. Even God was interested in being here, in this place, on earth. Not just in Heaven.
The grievers in your life are thankful for the promise of heaven. But that doesn't erase their sadness.
Third step to support a griever: Sit down
The most ancient part of the Hebrew scripture focuses on death, dying, and grief.
The book of Job (pronounced with a long “o”).
Job’s family and friends all died--in one day. He lost everything except for his wife and a few friends.
Our story picks up when the friends come to visit Job.
They did five things right.
They:
Made a plan
Went to see Job
Sat down
Were silent, and
Wept out loud
In this email, let’s consider their third right move.
They sat down.
In a 2011 study, the University of Kansas Nursing Department discovered the following:
Patients perceived the provider [the doctor] as being present at their bedside longer when he sat. Even though the actual time the physician spent at the bedside did not change significantly whether he sat or stood. Patients with whom the physician sat reported a more positive interaction and a better understanding of their condition.
All of our chaplains visit a lot of patients at our large hospitals. But some time ago, one stood out among the others. He was regularly visiting 80, even 90 patients in an 8-hour shift. To be fair, he usually worked what we call the “rounding shift” where seeing patient after patient is the focus. But no one came close to his numbers.
I became concerned. Success in caring for the spiritual needs of the sick is not measured by the speed at which it is accomplished.
So, I asked him. “John, tell me about your visits when you are on the rounding shift.”
“I go in. I sanitize my hands. I introduce myself. I ask if I can sit down. If they say yes, I pull the chair up close to the side of the bed. I look them in the eyes and listen for a little while. I ask if they need prayer. I wish them well. I sanitize my hands again, and I head to the next room.”
Perfect. Although looking at his numbers, I was concerned, I guarantee the patients didn’t feel rushed when this compassionate, older man sat and looked into their eyes.
And, to be overly practical, it has a lot to do with sitting down.
Eliphaz and Job’s other two friends must have referenced the University of Kansas study. Or else, they must have intuitively been able to feel that since Job was in such rough shape, they needed to sit with him—literally.
So support a griever, sit down with them-literally.
The first step to support a griever: Make a Plan
The most ancient part of the Hebrew scripture focuses on death, dying, and grief.
The book of Job (pronounced with a long “o”).
Job’s family and friends all died--in one day. He lost everything except for his wife and a few friends.
Our story picks up when the friends come to visit Job.
Initially, they did five things right.
They:
Made a plan
Went to see Job
Sat down
Were silent, and
Wept out loud
In this email, let’s consider their first right move.
They made a plan.
The scripture says they set out from their homes and met together by agreement to go and sympathize with Job and comfort him.
The first thing you can do for a griever is to gather a few other friends, meet together, and make an agreement to go and sympathize with them and comfort them.
Simple, yet often we don’t do it. I can count on one hand the number of times I’ve done this. But it’s so powerful.
To support a griever, maybe you need to start by gathering a group and making a plan.
This.Is.Hard
I used to say, “I’m sorry for your loss.”
Most people are polite when they hear it.
It’s better, I suppose, than never saying anything.
Then one friend said, “I hate that phrase.” Here’s what’s true: this moment is hard. You know that. And more than a vague apology for something that no one could control, you may need someone to acknowledge that this is hard.
Breathing is hard. Thinking is hard. Imagining the next few years is hard. Remembering anything is hard. Being polite is hard.
You can fill in some of your own hard things.
And now isn’t the moment for saying. “But other people have it worse.” Other people have hard things, too. And we can acknowledge that. But their hard moments don’t suddenly make this moment easy for you.
Try something.
Say “THIS is hard.”
Say “This IS hard.”
Say “This is HARD.”
And as you say it, know that I agree with you.
This is hard.
Tip #7: Never assume that you know what God will do
I’ve made this mistake in both directions.
I’ve been sure that a person is at the end of their life and they lived for several more years!
I’ve also been sure that a patient is fine and they have died shortly thereafter.
Let me tell you a story.
Less than twenty-four hours ago, I was in a hospital room with a family. They were gathered around the patient’s bed. Several children, their spouses, and the patient’s spouse made a semi-circle around her. I stood behind them, handing out tissues. The care team was preparing to remove her ventilator. The family was there to say goodbye.
The pastor from the patient’s church stood in the front of the family, at the foot of her bed. He tried to maintain silence after entering the room, but he didn’t survive five minutes.
He read scripture about not being troubled and how we would all be together again in heaven. He prayed a long prayer about God welcoming her into eternity and rejoicing that she would receive the promise of eternal life that very day. His prayer was a goodbye message.
The problem?
She's still alive. The care team removed the vent just after the pastor’s prayer. The family stood and watched and waited for their mother and wife to enter eternity. But, as I write these words, she is still breathing. Still struggling. Her last breath will likely come soon, but who knows? Only God knows.
That's why I try to never assume I know what God will do.
Never do this when you visit the hospital
Tip #6. Never assume that you understand
Maybe you had an aunt who had cancer.
That does not mean that you understand what every cancer patient feels.
Even more painfully, just because your dad died doesn’t mean that you fully understand when a friend loses her dad.
Never say, “I know how you feel.”
You don’t.
Instead, you could say, “If I were you, I might feel scared.”
That communicates that you are trying to put yourself in their shoes, not just giving advice you think they need.
Never assume that you understand.
Never do this when you visit a hospital
Tip #2 Never be afraid to cry.
When people hear what chaplains do, they ask some common questions.
One question is, “Do you ever cry when you are serving a family whose loved one just died?”
The answer, of course, is yes.
The day that violence, sickness, cancer, miscarriage, stillbirth, strokes, heart attacks, and death can no longer bring tears to our eyes is the day we should quit being hospital chaplains.
While it is important that I don’t make the situation about myself and my own sadness, shedding some tears with the family can build a meaningful bridge.
I no longer apologize for crying, and neither should you.
Never be afraid to cry.
Always do this when you visit the hospital
Tip #5: Just Listen (Shut up, please)
Being silent in the presence of another is a skill you must develop.
It’s quite difficult. But like other difficult skills, it can be learned.
After you’ve greeted the patient, you will feel the urge to say something.
To make sense of the situation.
To ask questions.
To remind them of the promises of God.
Remaining silent can feel like drowning.
Your brain twitches, “I’ve got to say...something!”
If you feel you need to say something, try this:
Count slowly from ten to one.
Take a deep breath.
Then do it again.
Pray a silent prayer. Be mindful. Be present.
The patient might be in pain, on medication, or just in deep thought about their situation.
Blurting a few words that make you feel better and rushing out the door won’t help.
Always practice silence and listening when you visit the hospital.
If you fail at holding silence, forgive yourself and try again.
If I had to sum up how to talk about death, dying, and grief in two words, they would be:
Listen well.
Always do this when you visit the hospital
3. Sanitize Your Hands
Nurses and other health care workers sanitize their hands dozens of times a shift.
You should be no different.
This is the most basic aspect of good health care.
While I know that “wash your hands” sounds more like a grandmother’s advice than it does good care for the sick, dying, and grieving, good hand hygiene does more than prevent disease.
It communicates respect.
It says to the person, “I value you enough to be sure I am not bringing in anything that could harm you further.”
I spray the sanitizing foam onto my hands as I walk into a patient room. Then, I make sure I am still rubbing the solution through my fingers when I approach the patient.
After all, I will certainly want to clean my hands on the way out.
If the patient sees me using the sanitizer only when I walk out, what am I communicating to her?
She may feel that I value my own health more than I value hers.
Health care has a saying: “Clean hands in, clean hands out.”
You should always do the same.
What NOT to say to a griever (Tip #2)
2. God needed another angel in heaven
First of all, there isn't any evidence in the Hebrew or Christian scriptures that this actually happens.
People don't become angels.
And being an angel isn't better than being a person.
Being a human being is the best it gets unless you are God.
Besides that, while the image of a placid-faced winged cherub invisibly fluttering around you with the spirit of your dead loved one is comforting to some, it is not comforting to all.
Finally, what kind of God needs to kill people or let them die?
Remember, it’s better to be quiet than to brush off the situation with a cliche.
What TO Say (Tip #8)
#8. Say, "I have time."
If you support a person in grief, they might be scared to burden you with their thoughts and feelings.
I didn’t do it on purpose, but earlier this week, I told three people in one day that if they wanted to talk that I had time.
One was saying goodbye to his mother in an ICU room.
Another was in a surgery waiting area for his spouse.
And the third was just having a down morning.
One of the three took me up on the offer. When we talked on the phone later about another topic, I circled back around and asked how he was doing.
Because I said "I have time", he shared more than he would have otherwise.
Obviously, you have to mean it.
You have to actually have time or be willing to make the time.
If you can’t, that’s ok. In that case, try, “This is really important. I really want to hear about how you are doing. Can we talk on Tuesday afternoon? I’ll clear my schedule and make sure I give you all the time you need to talk about Stephen.”
Some of the phrases in the first list of what NOT to say roll off the tongue more easily than the phrases in the second list.
They are, after all, clichés.
That means that we need to practice more helpful phrases. Please do that now.
I’m sorry Stephen died
I don’t fully understand, but I think God does
This feels wrong because it is wrong
What you are feeling is normal
This person will always be a part of your life
I’m with you
You have options
I have time
These will become more natural for you as time goes on, and you will become more helpful to a grieving friend.
What TO Say to a Grieving Person (Tip #4)
4. What you are feeling is normal
Kristen and I led a live online event around the topic of miscarriage and stillbirth. I asked participants to type in the chat emotions that a mom might feel when losing a baby. They listed emotions like:
Sadness
Embarrassment
Confusion
Anger
Guilt
Lostness
Envy
Unbelief
“It’s not fair,” and
Gratitude
All of those feelings are normal.
And we can affirm all those feelings in a grieving person.
No feeling should be considered wrong or discouraged.
It might make me more comfortable if the person is sad instead of angry; grateful instead of envious.
But it’s not about me.
If the person feels anything short of suicidal (a different topic altogether), we can affirm those feelings as normal. Do NOT try to talk them out of their feelings.
"What you are feeling is normal."
What to say to a Griever
Tip #1
1. Say "I’m sorry Stephen died."
This short statement has three positives.
1. It acknowledges what happened. It wasn’t just a “loss” or “hard time.” Someone died. And nothing compares to that.
2. This phrase names the deceased. When a person dies, their name vacates our vocabulary. Never again will we say, “Stephen called yesterday,” or “I’m making dinner when Stephen gets home,” or “Stephen, can you please take your laundry upstairs.” Because of this, people who loved Stephen feel an ache.
Their hearts can feel the discontinued use of his name.
When you say their name out loud in this phrase, “I’m sorry died”, you honor their life.
3. This phrase communicates that you are also sad this happened. Not in the same way as those closest to him, but in a parallel way.
It communicates that you wish he hadn’t died.
That wish is at the core of their experience of grief, and they will appreciate hearing you identify it.
Say, “I’m sorry died.”
What NOT to say to a griever (Tip #1)
What is the most common hurtful cliche said to people in grief? So famous that Kate Bowler wrote a book about it?
“Everything Happens for a Reason”
Now, I’ve said it before, too.
Don’t feel ashamed.
But put yourself in their shoes.
If a woman’s baby just died, how is she supposed to respond if you walk in, smile, and say “I know this is hard, but it’ll be okay. After all, everything happens for a reason”?
You are saying “There’s a good reason for your baby’s death.”
That belittles her sense of loss.
Even if you believe this, STOP saying it today!
In fact, you should say the opposite.
This doesn’t make any sense, I am so sorry.
I sure wish this hadn’t happened to you.
You don’t deserve this.
Stop saying Everything Happens for a Reason.
Some things are senseless and unREASONable.
And it’s okay to admit that, especially when you are talking with a person in grief.
